4 - 8 years ...
What is happening in your child's mouth around this age?
- By age 4 years the muscles of the face, lips and jaws have differentiated out into more complex and isolated movements.
- They can now isolate out the tip of the tongue and are able to articulate complicated words, keep all food inside mouth when eating as well as licking food from around the outer edges of their mouth. Their tongue should be able to reach all the teeth to clean debris from food off—even the back molars.


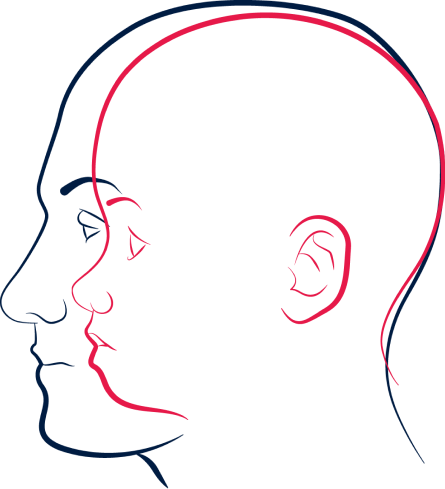
Imagine the face and jaw as a tent.
The tent with it’s tent poles is useless without the guy ropes as they provide the tension to hold the shelter straight and strong. The guy ropes of your face are the muscles. In particular, the muscles of the lips, face and tongue. If we have the right tension in these muscles the forces acting on our face tend to be more balanced. In the growing face especially, these forces contribute to bone growth via the pull of the muscles on the bone.
This is a great system, provided the tensions on the ropes are correct. In muscle terms we call this “length tension relationships”. In the face, things such as pacifier use, thumb sucking, open mouth breathing and nasal obstruction can alter the length tension on these muscles. This can result in incorrect growth forces.
- By age 4 years they have lost the round face and have developed more vertical height through the lower third of the face.
- Speech is complex and articulation is clear.
- Eating all different food groups and textures and sizes.
- Teeth- all 20 primary teeth should have erupted and be meeting in a balanced occlusion.
- Sleeping- your child should be sleeping quietly through the night and wake well rested. Sharon Moore’s book, ‘Sleep Wrecked Kids’ is a great resource, if they are not sleeping well.
- Around 6-7 years of age your child will start to lose their baby teeth and we will see the beginning of the eruption of the permanent dentition.
- Parents will still need to clean children’s teeth as they are not yet dexterous enough to do it well.

This is the time to take your child to a dental professional to ensure that they are developing good oral hygiene habits. Shereen Lim’s book ‘Breathe, Sleep, Thrive’ is another fantastic resource to have on hand
Get the bookFor those looking to improve their child’s facial growth and avoid major orthodontic interventions it is going to be essential that you are working alongside a Dental practitioner.
They will track their progress using Munchee with photographs and measurements to ensure that the natural forces of growth are being harnessed so that their teeth are coming into good alignment. Working with practitioners who are specialised in Oral Myofunctional Therapy (OMT) can play a very important role in ensuring children have optimal tongue, lip and face muscle function to optimise jaw bone growth and stability.
See the directory
How can a Munchee assist at this age?
- Most children simply do not eat food that requires a lot of chewing. Most food in modern living is soft and processed.
- 5 minutes of chewing every day for every child will assist their facial growth and development and oral hygiene.
- Myo Munchee is a great tool for keeping teeth clean and gums healthy- the small prongs massage the gums and clean the teeth.
- Munchee is a great oral motor exerciser for all children to activate and stimulate oral growth and optimise function- gym workout for the lips, face and jaws. There is much growth of the mandible occurring during this time (lower jaw bone) and the Munchee is a fantastic way to assist this growth.
Wolff’s Law:
Wolff’s Law states that your bones will adapt based on the stress or demands placed on them. When you work your muscles, they put stress on your bones. In response, your bone tissue remodels and becomes stronger. But Wolff’s law works the other way, too. If you don’t use the muscles surrounding a bone much, the bone tissue can weaken.

So, chewing a Munchee for 5 minutes everyday, will assist with facial growth and development because it is activating the growth centres of the bones of the face and jaws.
Which size Munchee is right for my child?
For this age group there are many things to think about when deciding which size Munchee is right for your child. Things like age and where they are at developmentally will play a big part, do they have some delay or are they low tone? Have they used a Munchee before?
What are the goals your wanting to achieve with the Munchee and are you working with a practitioner- they will make recommendations for you that may be different to the sizing chart.
If we are looking for optimal jaw growth we will be looking to move to next size as soon as possible for their age.
Read MoreFactors to think about for your child.
Use the sizing chart and measure the intercanine measurement as a general guide and cross match with the criteria below.
-
Body Size
Are they big or small for their age- their jaws are likely to match in with their overall size.
-
Jaw size
Narrow palate, crooked teeth, history of tongue-tie. This child will be better to start with a smaller appliance and transition to the next size once they are very comfortable.
-
Overall Tone
Do they have evidence of low tone? Do they have trouble keeping their lips together when eating, are they dribbling or drooling. Do they have low tone in their body as well. Start with a smaller size to ensure they can manage and then transition to the next size once they have achieved comfortable lip competence.
-
Special Needs
Does your child have a condition that has affected oral motor function? Advice from your practitioner will be helpful here but always tend to the smaller size to ensure that they can manage the device for best outcomes.
-
Have they used a Munchee before?
If they are confident and experienced with Munchee then we would recommend they use the bigger size for their age range.

Although the Myo Munchee Junior is suited to children aged 4+ years, there can be cases where your child will be ready to transition to the Junior earlier than expected, AND there can be cases where they will need to stay with the Mini longer.
The time to transition up to the next size, will be determined by their age and as how functional they are, as well as what goals you are wanting to achieve. Those with special needs will be guided by their practitioner when to move to the next size.

If they have been using one for some time, they should be comfortable with moving up to the Junior by age 5 years
Shop now
Important!
It is essential that your child is able to keep their lips together around the Munchee to be able to keep the jaws in the correct place as well as nose breathe and train the correct swallow pattern.
4 - 8 years
Signs and Symptoms
of Oral Dysfunction
- Dribbling and drooling
- Tongue thrust swallow pattern
- Imperfect bites and misaligned teeth
- Facial and jaw asymmetries
- Mouth resting open
- Mouth breathing
- Fussy, picky eater
- Sleep disturbance, snoring, nightmares, sleep walking
- Teeth grinding
- Delayed speech
- Ear infections
- Sinus congestion and venous pooling
- Behaviour and attentional issues
- Bed wetting Prolonged pacifier/dummy use or thumb/digit sucking
Which Practitioner should I
see for my child’s concerns:
see for my child’s concerns:
Low oral motor tone
Speech Pathologist, Occupational Therapist, Myofunctional Therapist, Chiropractor
Special needs children
with Downs syndrome and
CP- Speech, OT, MFT
Ear drainage
GP, Dental, Chiropractor, Osteopath
Mouth breathing
Specially trained therapists such as Buteyko Breathing therapists and all practitioner with training in Oral facial Myofunctional Therapy
Thumb Sucking
Transition tool thumb- sucking protocol using Munchee with Paediatric health practitioner, Dentist, Speech Pathologist, Myofunctional Therapist and Psychologist
Pacifier replacement
Parent supported by MFT or other health professional
Sign up for news and updates
Enter your details to receive news and updates on all things Munchee!
At any Age and any Stage, Myo Munchee can support you on your life's journey
Download your free copy of our eBook 'Why Children Must Chew'

Sign up for news and updates
Enter your details to receive news and updates on all things Munchee!
More About Munchee
How do I use a Munchee
Watch this video to find out the most important movements for chewing a Munchee
Watch videoResources
Please check out our resources for more information and shoot us an email if there are specific topics you'd like more info on!
View our resourcesContact Munchee
Got a question for us to chew over or need product and ordering support? Reach out to Munchee
Send messageFollow Munchee
FAQs
-
Relationship between chewing, speech, and the Myo Munchee
Speech is a fine motor task that requires muscle strength, movement, and co-ordination. Disordered speech patterns can develop to compensate for movement deficiencies. Research shows impairment in the structure and/or function of the articulatory muscles can significantly impact the production of sounds. The Munchee supports the development of the jaw, occlusion of teeth and tongue rest positions which may be impacting speech clarity. It may also promote strength and endurance of the of the articulators.
The Myo Munchee can support the strengthening, stabilisation, positioning of muscles for the promotion of correct swallow functions.
-
Why is tongue posture important?
Did you know that tongue position can impact everything from chewing and swallowing to the way we look and speak? Incorrect tongue posture can impact on swallowing patterns, jaw growth, tooth eruption and spacing.
Every time we swallow (that’s once or twice per minute!) the tongue pushes up to the roof of the palate and then backwards to complete an ideal swallow pattern. When a mouth breather swallows, the tongue tends to thrust forward instead of upwards and the lower jaw tends to move backwards instead of staying still. This creates forces that interfere with the position of the teeth and work in opposition to normal facial growth.
Orofacial Myofunctional Therapy helps mouth breathing in children by assessing the correct structural development of the face, teeth, and jaws of your little ones. The Myo Munchee is a powerful adjunct tool for OMT treatment plans.
-
Munchee Movement
The Munchee Movement brings parents, children and practitioners together with the common purpose of reclaiming natural, functional chewing and oral motor function. We are building the movement for positive change and a healthier world by bringing more awareness and empowering people and parents through new skills and knowledge in terms of:
Integrating facial, jaw and tongue muscles working together for better jaw function and breathing
Helping people to function better from birth to maximise healthy development
Connecting with a new generation of professionals who want more ways to help their clients with minimal intervention.
-
Relationship between swallowing and the Myo Munchee
The Munchee supports the development of swallowing skills in babies, children and adults including older populations. Disordered or poor swallowing includes:
- poor chewing skills (mastication)
- incorrect jaw positioning and movements
- overuse of lips, facial muscles, and cheeks
- excessive head movements and nodding
- tongue thrusting through lip and/or teeth
- coughing and choking
- excessive dribbling and drooling
-
How can I encourage my child to use their Munchee?
Attempting to incorporate Munchee time into daily routines, can appear overwhelming at first. However, it really comes down to repetition, positive encouragement, and frequent interactions every day - this is how people are finding success with their children. It hopefully then becomes habit and second nature.
Incorporating Munchee time into routine activities such as reading/tv/gaming time, bath/shower time, travelling in the car, etc. Many parents only allow TV or gaming time, when a Munchee is in their child’s mouth!
Plus there is also modelling…when a parent or older sibling is using their Munchee a little one will often happily engage with their own Munchee too.
The Munchee Moves are a wonderful way for children to incorporate their Munchee time, some movement, and family fun for all!
Try to ensure Munchee time is always fun, offered often but never forced.




























